If you’re dealing with frequent back or neck pain, your posture might be playing a bigger role than you think. Whether you're sitting at a desk all day or scrolling on your phone for hours,…
Your spine is composed of a series of spongy discs, which are sandwiched in between a tower of vertebrae. In a normal, healthy spine, these structures act as shock absorbers between these bones. This alignment not only gives the spine its much-needed flexibility but also its innate force of resistance. Unfortunately, as is the case with most mechanical systems, our discs wear down with time. Some people experience this degeneration with little to no issues. Others, however, develop a variety of health issues and adverse symptoms. Every individual has their own unique anatomy, which in turn affects the severity of symptoms.
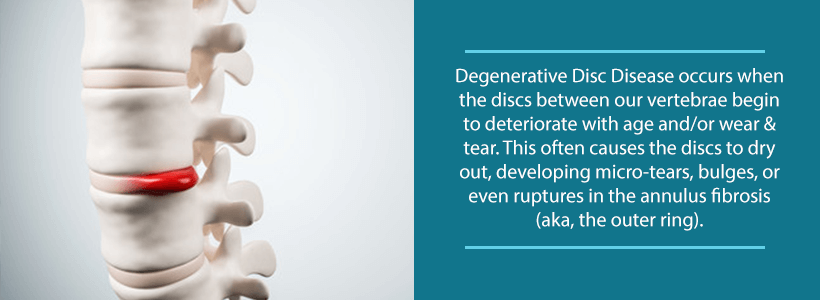
Spinal disc degeneration may occur in a variety of different ways. Most commonly, the discs simply dry out, which flattens them, inhibiting their function. Naturally, a flatter disc also means less shock absorption. In addition, this translates into less padding between the vertebrae, as well as pain.
In some cases, the hard outer shell of the disc may crack, causing the soft inner material to leak out. When this happens, it often applies pain-generating pressure to nearby nerves. Sometimes, the disc may also bulge or slip out of place, likewise inflaming nerve tissue.
Luckily, these are treatable problems that medication, physical therapy, steroid injections, and sometimes surgery can alleviate. Just know that if you have back pain, there are options for you. Always seek out medical assistance if your symptoms affect the quality of your everyday life.
Degenerative Disc Disease & Related Issues
Again, the discs of the spine act as impact cushions between the vertebral bones. In addition, our discs consist of a rubber-like structure that is made up of fibrocartilaginous tissues. The medical community calls the outer layer of an intervertebral disc the annulus fibrosus. Alternatively, doctors refer to the inner core of the disc as the nucleus pulposus. The latter is the portion of the disc that doctors describe as soft and jellylike.
Knowledge of this structure is paramount to understanding just how the discs of the spine degenerate, as well as what affects this process. We already know that discs may dry out over time, leading to less distance between the vertebrae of the spine. Additionally, we also know that changes in the disc’s structure may occur via cracks, tears, bulging, and so on. In some cases, the disc may even fracture into smaller pieces.
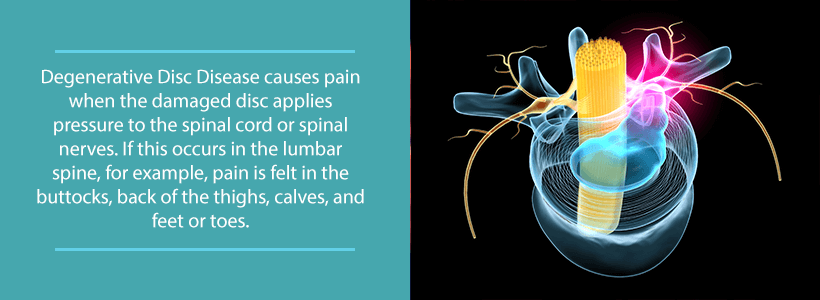
But, deterioration doesn’t just end there. When our body undergoes negative changes such as these, it tends to overcompensate in response. As a result of less padding between the vertebrae, the body produces osteophytes, otherwise known as bone spurs. These are bony projections that form on the perimeter of our bones. Unfortunately, this process may result in pressure against the spinal cord or adjacent nerves. This can inhibit the function of these nerves, leading to painful symptoms.
Degenerative disc disease may also cause cartilage breakdown. This poses a significant problem, as cartilage helps to reduce friction in the joints. Likewise, degenerated discs may also lead to herniated or bulging discs, as well as spinal stenosis. The latter here describes an instance in which the space surrounding the spinal canal narrows, potentially causing pain, weakness, and numbness.
Degenerative Disc Disease (DDD) Symptoms
It is vital to note that DDD will happen to some extent in almost everyone. However, not all patients will experience negative symptoms as a result. Yet, others will experience extreme pain which affects their ability to carry out daily tasks. Usually, degenerative disc disease begins with damage to spinal structures. However, over time, this may evolve into problems elsewhere in the body.
Symptoms of degenerative disc disease vary from quite mild to utterly incapacitating. Usually, the symptoms with the earliest onset are pain and weakness. You may notice that the pain tends to travel to other parts of the body. Over time, these symptoms may evolve into other conditions, such as osteoarthritis, which leads to even more pain and stiffness in the spine.
The location of the damage in the spine has a natural effect on the nature of the condition’s symptoms. For example, when DDD affects the lumbar spine, painful nerve symptoms and tingling may also arise in the buttocks, upper thighs, legs, and/or feet. Conversely, when the condition affects the cervical spine, symptoms may extend to the shoulder, arm, and/or hand.
Lastly, the body may try to overcompensate for structural instability through muscle spasms. Any of the pain that the condition causes may also be exacerbated during certain activities such as bending, lifting, twisting, or prolonged periods of sitting. Patients may be able to temporarily combat this by walking or lying down.
Degenerative Disc Disease (DDD) Diagnosis
Doctors often begin their diagnostic process with a series of questions that probe the patient’s medical history, prior injuries, and familial trends. Your doctor will also ask questions about the location of symptoms, as well as which activities result in pain. During a physical examination, your doctor may look for the following:
- Muscular Symptoms: The doctor will look for any signs of muscle weakness, atrophy, or abnormalities in movement.
- Pain Triggers: The doctor will ask the patient to perform specific motions in order to figure out which areas the condition is affecting. He or she may also apply pressure to certain areas to determine the existence of degenerated discs.
- Reflexes: Utilizing a reflex hammer, the doctor will test your nerve function to see if there are any compressed nerve roots. In some instances, your doctor may apply heating and cooling techniques to see if the nerves react properly to adjustments in temperature.
Your doctor may also deem it necessary to order diagnostic imaging tests, such as a CT or MRI scan. He or she may also use a discogram, which utilizes dye injections to locate the disc that causes pain.
Degenerative Disc Disease (DDD) Treatment
Treatment for any medical condition typically involves either conservative methods or surgery. Most of the time, doctors prefer to use nonsurgical methods, as these typically end up being sufficient. That being said, there are certainly more severe cases of DDD in which surgery becomes absolutely necessary.
Conservative treatments for DDD include physical therapy, occupational therapy, medications, and weight loss regimens. Doctors may also opt to use steroidal facet joint injections to provide their patients with temporary yet effective pain relief. Sometimes, doctors recommend back braces for patients who struggle with spinal instability. There are also minimally invasive procedures available, including radiofrequency ablation as well as heated catheter insertion.
If the patient does not respond to conservative treatments within 12 weeks, then the doctor will begin to consider surgery. Generally speaking, there are two options that surgeons commonly employ to treat degenerative disc disease. Most commonly, surgeons use spinal fusion to weld two vertebrae together, permanently increasing spinal stability. In other instances, a surgeon may use decompression surgery to remove a portion of the offending joint, relieving adjacent nerve pressure.
Contact Us
Are you experiencing back pain that doesn’t seem to go away on its own? If so, contact Orthopedic & Laser Spine Surgery today at (855) 853-6542. Our facility is staffed with only the most passionate experts who put the patient’s needs above all else. It is our goal to ensure that every patient is given an individual care plan that best suits the specifics of his or her case. You don’t have to live in constant discomfort. Contact us today and begin your journey toward pain-free living!