Back and neck pain can be debilitating, significantly impacting your quality of life. If conservative treatments like physical therapy, medication, or spinal injections haven’t worked, you might be considering surgical options. One increasingly popular and…
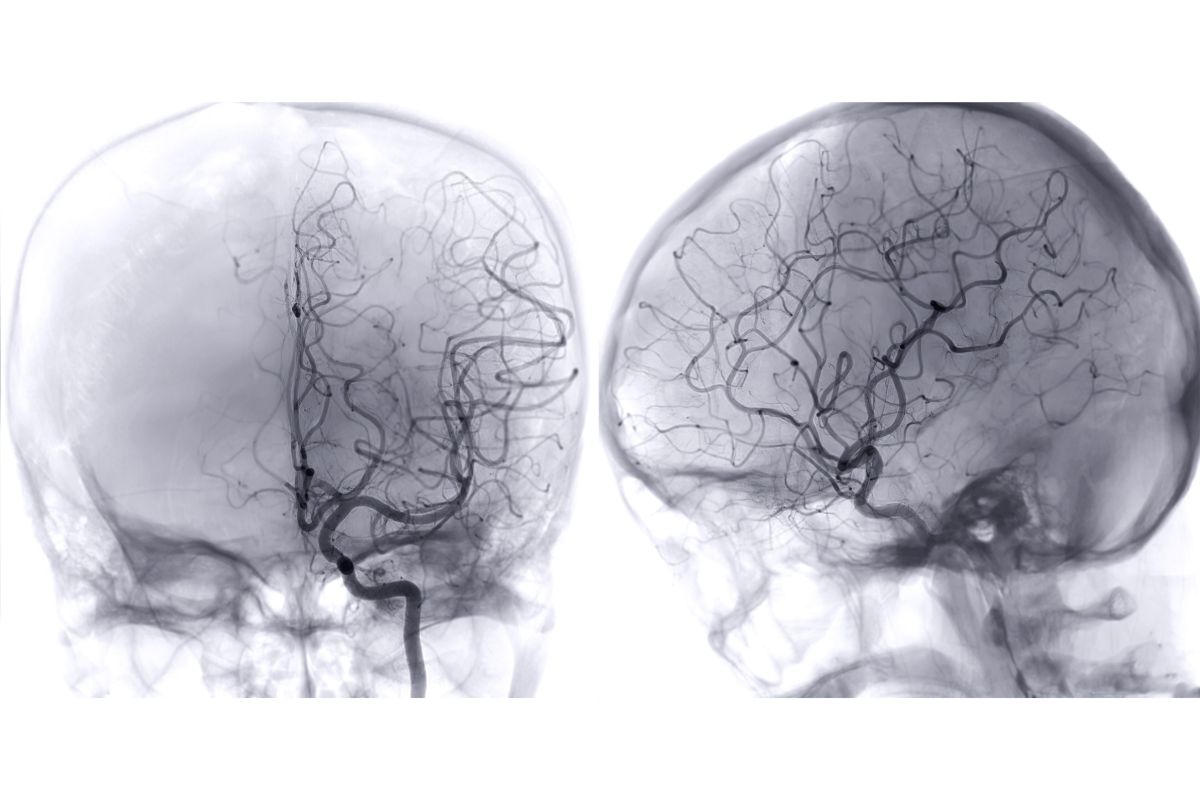
Introduction: Perioperative cerebrovascular accidents (CVAs) related to spine surgery are infrequent, yet they can result in considerable disabilities. There is a pressing need for further studies on spine surgeries to identify patients who are at risk of experiencing perioperative CVAs. A retrospective descriptive study coupled with a meta-analysis was conducted to evaluate the characteristics and outcomes of patients who suffered CVAs during spine surgery.
Methods: A retrospective analysis was performed on patients aged 18 and older who underwent spine surgery under general anesthesia at a hospital from April 2011 to March 2023. Initially, 2,391 patients were identified, from which 2,346 were included after excluding 45 individuals who underwent debridement for surgical site infections. A meta-analysis, incorporating data from the present retrospective study, was subsequently conducted. Relevant databases, including PubMed and Google Scholar, were searched for original, peer-reviewed articles published in English.
Results: Among the 2,346 patients included in the study, four (0.17%) individuals—comprising three men and one woman—experienced perioperative CVAs associated with spine surgery. The types of CVAs varied significantly: one instance involved a cerebral hemorrhage attributable to dural injury sustained during posterior occipitocervical fusion. Two cases of cerebral infarction were reported following lumbar laminectomy and anterior thoracic fusion, linked to the discontinuation of anticoagulant therapy. Additionally, one case of posterior reversible encephalopathy syndrome occurred after microscopic lumbar discectomy due to gestational hypertension. The subsequent meta-analysis encompassed three studies with a total of 186,860 participants. This analysis identified multiple risk factors for perioperative CVAs, including surgical intervention at the cervical level (pooled odds ratio [OR]=1.33), hypertension (pooled OR=2.27), atrial fibrillation (pooled OR=8.78), a history of heart disease (pooled OR=2.47), and diabetes (pooled OR=2.13).
Conclusions: The analysis suggested that the potential risk factors for the four cases of perioperative CVAs documented in this study included intraoperative dural injury, the preoperative discontinuation of anticoagulants, and a history of gestational hypertension. Furthermore, the meta-analysis indicated that undergoing cervical spine surgery, along with existing conditions such as hypertension, atrial fibrillation, heart disease, and diabetes, significantly heightens the risk of CVAs. This underscores the critical importance of thorough risk assessment, preoperative optimization, and diligent postoperative care to mitigate the likelihood of spine surgery-associated perioperative cerebrovascular accidents.