Back and neck pain can be debilitating, significantly impacting your quality of life. If conservative treatments like physical therapy, medication, or spinal injections haven’t worked, you might be considering surgical options. One increasingly popular and…
The prevalence of fractures caused by osteoporosis is increasing due to rising life expectancy, significantly impacting the quality of life among the elderly population. These fractures are both a disease and an injury, prompting a shift from exclusively conservative treatment methods to the incorporation of newer techniques and implants, which expand the indications for surgical interventions. This article outlines current treatment options for osteoporotic fractures.
Globally, fractures due to osteoporosis have reached epidemic levels. In the USA, the elderly population with osteoporosis is expected to rise by 32% between 2010 and 2030. Data indicates that the prevalence of spinal vertebral fractures in individuals over 40 years is 5.4%, escalating to 18% in those over 80 years. Vertebral compression fractures (VCFs) can precipitate a cycle of pain and immobility, exacerbate comorbidities, impair respiratory function, and increase mortality risks, which can reach as high as 90% over a seven-year span in the very elderly.
Osteoporotic thoracolumbar spinal fractures account for approximately 20% of all osteoporotic fractures and are significant contributors to morbidity among older adults. These fractures often lead to severe pain, deformity, and mobility issues, drastically affecting the individuals’ quality of life. Originally, conservative management was the primary approach to treat these fractures. However, advances in minimally invasive surgical techniques have prompted interest in surgery as a viable option.
Bone strength is a multifaceted attribute influenced by bone mineral density, turnover, remodeling, and the intricate arrangement of the bone matrix. Additionally, it is determined by the mineralization rate, collagen denaturation, and the ability to repair microfractures. The fracture occurrence in osteoporotic patients can be viewed as a combination of accidental injury and underlying disease processes, which affect bone integrity and strength.
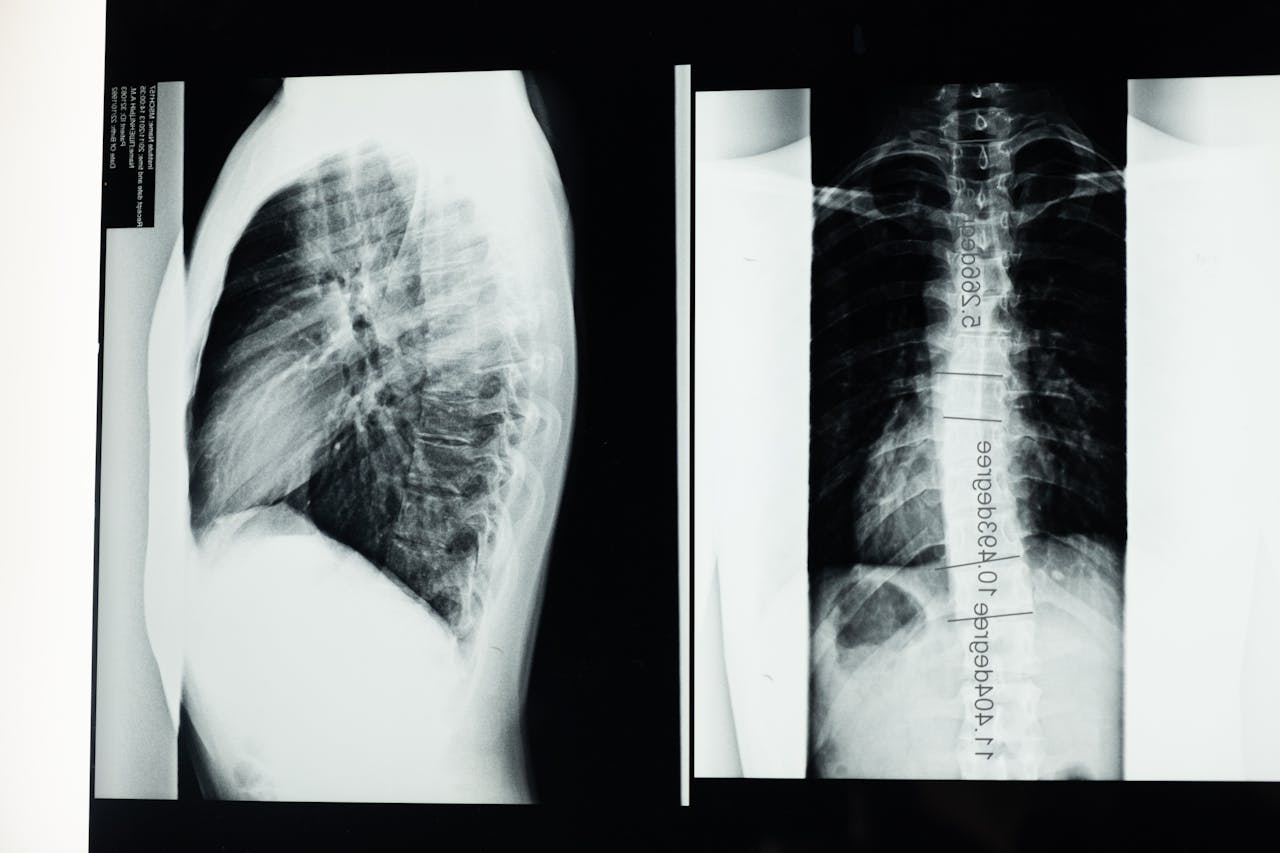
The spinal vertebrae primarily endure compressive forces and are also subjected to bending and stretching forces. Daily activities and body weight contribute significantly to the loads placed on these structures. As osteoporosis progresses, the vertebrae undergo porosity changes, which lead to deformities either gradually or following a sudden effort. This loss of structural integrity manifests in various fracture patterns: compression, wedge, and biconcave fractures, with wedge fractures being the most prevalent form.
Recent studies suggest that upwards of 60% of spontaneously occurring thoracolumbar spine fractures are initially asymptomatic. When conventional radiography fails to reveal traumatic deformities, MRI is employed to detect these occult fractures. Elderly individuals may sustain a fracture from minimal external forces, such as falls from standing height, supporting the notion that bone strength is crucial in fracture development even without a traumatic event.
The classification of thoracolumbar spinal fractures, such as the AO spine classification system, aids in diagnosing and determining treatment approaches. This system categorizes fractures based on the direction of the force applied and the structural integrity of the vertebra, with subdivisions for varying degrees of injury. The German Association for Traumatology and Orthopaedics (DGOU) further tailors classifications based on imaging findings, detailing involvement of the vertebral body and posterior wall integrity.
Traditionally, management of osteoporotic thoracolumbar spinal fractures has involved conservative treatment strategies, including analgesics, early mobilization, and physical therapy. However, when conservative measures fail to provide relief or when the fracture’s structural integrity is substantially compromised, surgical intervention may be warranted. Stable type A fractures typically progress with conservative measures, while those with significant angular deformities may require surgical correction.
Balloon kyphoplasty (BK) and vertebroplasty (VP) are two minimally invasive surgical techniques gaining traction in treating osteoporotic fractures. Although the popularity of these methods declined following initial skepticism regarding their efficacy, subsequent studies have validated their effectiveness in alleviating pain and improving patients’ quality of life. BK utilizes inflatable balloons to restore vertebral height before cement stabilization, whereas VP involves direct cement injection into the fractured vertebra.
Both procedures, performed under local anesthesia and conscious sedation, present several advantages, including reduced postoperative complications and outpatient recovery. However, they are not universally applicable, as patients with severe spinal deformities or multiple fractures may require more extensive surgical solutions.
In complex cases, combining BK and posterior spinal instrumentation may offer a comprehensive treatment approach. This combination is particularly beneficial when addressing spinal deformities or multiple fractures, as BK can rectify vertebral height while instrumentation provides structural support, mitigating the risk of future fractures.
In conclusion, the growing incidence of osteoporosis-related fractures necessitates a multifaceted treatment approach. While conservative management remains the first-line option for many patients, surgical interventions such as balloon kyphoplasty and vertebroplasty have proven effective for those with significant pain and mobility issues. Ongoing advancements in minimally invasive techniques are enhancing treatment outcomes, providing elderly patients with improved quality of life while reducing potential complications associated with traditional surgical methods.