Traveling in a car, train, or airplane and trying to sleep while sitting in an upright, cramped position can cause your back and neck to be positioned awkwardly, causing back, shoulder, and neck pain. However,…
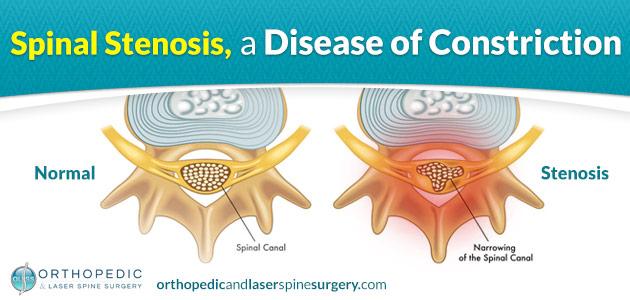
Spinal stenosis is a condition that affects the spinal canal reducing the amount of space available for spinal nerves as well as the cervical spinal cord. Because the spinal cord is not present in the lumbar section of the spinal canal, compression of the spinal cord is not a worry when spinal stenosis affects the lower back.
Examining Spinal Stenosis
Spinal stenosis is a condition that affects the spinal canal reducing the amount of space available for spinal nerves as well as the cervical spinal cord. Because the spinal cord is not present in the lumbar section of the spinal canal, compression of the spinal cord is not a worry when spinal stenosis affects the lower back. If the spinal cord is being compressed this condition may also be referred to as cervical myelopathy and may require immediate decompression depending on how severe the compression is.
What causes Spinal Stenosis?
Conditions that develop and take up space in the spinal canal are generally responsible for spinal stenosis. Bone spurs, herniated disc material, as well as excessive ligament growth are usually the culprit, but other more rare conditions such as a spinal tumor or cyst may also be to blame.
Treating Spinal Stenosis
If a condition is causing inflammation that is pushing into the spinal canal is to blame, often anti-inflammatory medication and treatment of the underlying condition is all that is required to resolve the condition. Physical therapy that puts an emphasis on strengthening core muscles that provide support for the spinal column is a common form of therapy. In some instances where inflammation is not being reduced by oral methods, a corticosteroid injection may be delivered to the injured site through an injection. This will help target the area with a stronger anti-inflammatory and should provide much better results.
Treating Spinal Stenosis through a Surgical Approach
If after 2 – 3 months of conservative non-surgical treatments fail to yield favorable results, surgical intervention may be the patient’s last form of relief. The type of surgery that is required will depend on what underlying condition is causing the stenosis. In the case of a herniated disc, a procedure call a discectomy could provide the patient with significant relief.
The Discectomy Procedure
The goal of a discectomy procedure is to gain access to a damaged vertebral disc, remove the herniated material, and if needed provide support to the area to allow the disc to heal and help prevent from future disc herniation. A traditional open back discectomy will require a large incision, general anesthesia, stay in a hospital for 1 – 3 days, depending on whether complications arise or not, and a 2 week to 1-month recovery. If a spinal fusion is required to stabilize the spine after the discectomy, a longer stay in the hospital will be required, and recovery time will increase drastically.
Is there a Better Approach to a Discectomy Procedure?
Depending on the size of the disc herniation the patient may elect to take a much easier approach to the surgery. Through an endoscopic discectomy, the surgeon will only need to make an incision about the size of a postage stamp, general anesthesia will not be required, and barring complications, there is no stay in the hospital. The procedure is performed in an outpatient setting with the patient being allowed to leave after a few hours of post-surgery monitoring. Because this revolutionary form of surgery does not require cutting or tearing of the soft tissues and muscles, recovery is very quick; patients who undergo endoscopic discectomy surgery are usually back at work within 1 or 2 weeks.
Are you a candidate for an endoscopic discectomy? Follow the link in the image below to use Atlantic Spine Center’s free online tool. It only takes a few minutes of your time and may save you months worth of recovery time.