If you’re dealing with frequent back or neck pain, your posture might be playing a bigger role than you think. Whether you're sitting at a desk all day or scrolling on your phone for hours,…
Those who are seeking degenerative disc disease treatments have probably come across facet nerve ablation in their searches. But, is this an effective method of treating your degenerative disc disease symptoms?
For many, facet nerve ablation reduces painful symptoms much longer than conservative treatments or medications. But, how exactly does it work?
Before we delve into the specifics, let’s take a closer look at degenerative disc disease and how it causes discomfort.
A Quick Look at Your Spine
Your spinal column, made up of 33 vertebrae, houses the spinal cord and helps support the body and its many movements. The spinal column is divided into four main regions:
- Cervical (neck)
- Thoracic (chest/upper back)
- Lumbar (lower back)
- Sacral (pelvic region)
Of course, the spinal column is more than just a series of bones stacked upon each other. A complex system of muscles, tendons, ligaments, facet joints, and intervertebral discs support the spine and allow nerves to branch out from the spinal cord. Furthermore, all of this structure enables the brain to communicate effectively with the rest of the body.
Unfortunately, despite the major responsibilities of the spine, it is nonetheless prone to injury. This can be due to poor personal habits, the effects of aging, or trauma to the area. For instance, when the spine’s structure is altered, it can compress the nerves exiting from the spinal column. This can lead to painful and debilitating conditions that require immediate treatment.
What is Degenerative Disc Disease?
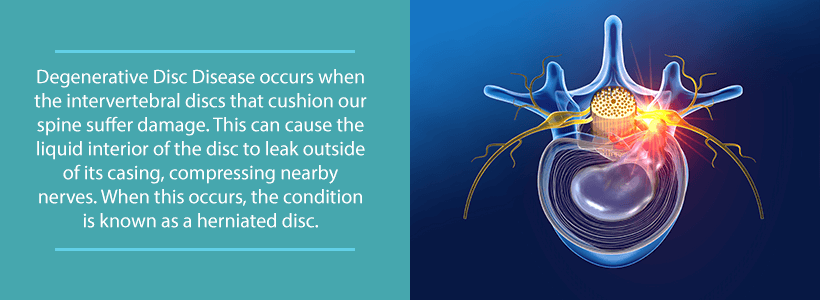
In between most of your vertebrae are circular discs that absorb the shock of your everyday movements. Intervertebral discs consist of a tough outer layer surrounded by a gel-like inner layer. As we age, these discs begin to dry out and lose their shape. In some cases, this can cause pain, spinal instability, and other neurological symptoms like burning or reduced sensation.
But, the degeneration of our discs is not actually a disease. Yes, despite the name.
Degenerative disc disease is somewhat of a misleading label. It’s intended to be descriptive of the natural erosion of the discs resulting from wear and tear. As such, disc degeneration is most common in the neck and lower back. Why? Because these areas must cope with the greatest amount of stress while you go about your daily life.
Does degenerative disc disease mean that the pain will get worse as you get older?
Not necessarily.
“Degenerative” refers to the degrading of the disc—not the worsening of symptoms. You may be surprised to find out, in some cases, that symptoms actually improve over time. This is known as the degenerative cascade.
In a nutshell, this means, at first, you may experience painful symptoms that limit your function. Over time, however, the instability of the disc and surrounding vertebrae can lead to back or neck pain that comes and goes. Then, as this portion of the spine re-stabilizes itself, pain becomes less frequent. Of course, this doesn’t happen overnight. The entire process can take up to thirty years.
Thirty years is obviously a long time to wait for pain relief.
Luckily, there are several degenerative disc treatments that can manage symptoms and stabilize the area.
Let’s take a look at some of the common degenerative disc disease symptoms that you may be experiencing.
What Does Degenerative Disc Disease Feel Like?
In many cases, degenerative disc disease occurs in the neck or lower back. These areas of the spine have more flexibility to support the body’s movements. Generally, those who are dealing with degenerative disc disease feel continuous, low-grade pain and occasional flare-ups of severe pain. Acute bursts of pain can be due to bouts of recent activity, but sometimes the cause may unknown.
In addition to the pain, you may experience:
- A “giving out” or “locking” feeling. This could feel like the neck or back is not strong enough to support your movements.
- Muscle spasms or tension. As mentioned earlier, the spine and nearby muscles are connected. Instability of the spine can affect the functioning of these muscles.
- Radiating pain. If a nerve is compressed or injured due to spinal instability, you may feel sharp, stabbing pain in other areas of the body. For example, a damaged disc in the neck can lead to pain in the shoulder, arm, or hand. Lower back degeneration may cause pain in the hips, buttocks, and down the leg.
- Fluctuating pain while holding or changing positions. Those who change positions frequently may experience less pain. Conversely, sitting or standing for long periods of time can worsen lower back pain. Also, reading or using mobile devices for extended periods of time can cause a spike in neck pain.
The severity of chronic pain will vary from person to person. Some individuals feel little to no baseline pain. Others may deal with severe, disabling pain.
So how can you get pain relief? Let’s look at some options.

Conservative Degenerative Disc Disease Treatments
There are some self-care approaches that you can take to manage degenerative disc disease pain at home. The goal of these treatments is to reduce pain, thereby making your daily activities more tolerable.
Here are some things you can do:
- Heat therapy. A warm bath or heating pad can reduce muscle tension and spasms. The heat relaxes nearby muscles and also increases blood flow to the area.
- Icing the area. A cold pack can aid with pain relief by reducing inflammation. If you experience a pain flare-up after exercising or physical activity, try icing the area.
- Over-the-counter medications. Before trying more powerful and potentially habit-forming prescription drugs, consider over-the-counter pain medications. Non-steroidal anti-inflammatory drugs like ibuprofen can reduce pain and inflammation in the affected area.
- Manual manipulation. A chiropractor, licensed massage therapist, or another spine specialist can manually adjust the spine. As a result, you may experience temporary pain relief and more movement to the area.
- Exercise. Keeping the muscles near the spine healthy and flexible assists in supporting the spine. A physical therapist can help you develop an exercise routine that improves the strength and flexibility of your neck and back.
Have you tried these degenerative disc treatments with little or no success? Maybe it’s time to consider facet nerve ablation.
What is Facet Nerve Ablation?
Your nerves send and receive information to the brain. This includes alerting the brain that something is wrong by sending pain signals. For example, if you put your hand under scalding water, the pain signals tell you to quickly remove your hand. This rapid response is designed to prevent major injuries.
Facet nerve ablation—or radiofrequency ablation—uses a needle to create a heat lesion on a pain-transmitting nerve. The lesion prevents the nerve from dispatching pain signals to the brain. Moreover, this minimally invasive procedure is relatively safe with few side effects.
But, nerves are important. Right? So, why would we want to injure or stun them?
In the case of degenerative disc disease treatment, facet nerve ablation has important advantages. It may be a long-term solution to managing pain which decreases the need for strong—and potentially dangerous—pain medications. In some cases, radiofrequency ablation can help reduce neck and back pain for up to six months or sometimes even longer.
This reduction in pain can allow you to participate in (and stick with) a physical therapy or rehabilitation program which ultimately increases your strength, flexibility, and range of motion. So, as the effects of radiofrequency ablation gradually wear off, you still can become stronger and have more stability in the spine.
What Happens During Facet Nerve Ablation?
Facet nerve ablation lasts up to 90 minutes. What happens during this time? Let’s take a look at the procedure.
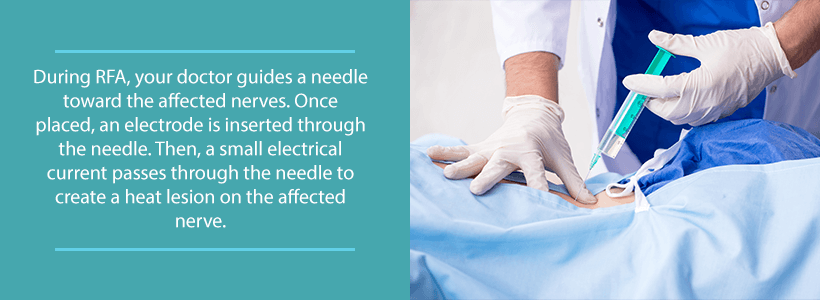
You will be asked to lay on your stomach during the procedure. In some cases, you may be given mild sedation, but you will be kept awake during the procedure. This allows you to describe what you are feeling during the stimulation and lesioning of the nerve.
Using a small camera, the doctor guides a radiofrequency ablation (RFA) needle toward the affected nerves. Once placed, an electrode is inserted through the needle. A small electrical current then passes through to the target nerve. This stimulates the nerve and briefly recreates the symptoms you tend to feel. Once the target nerve is confirmed, a heat lesion is created on it. This can be performed by different RFA methods including:
- Conventional: Continuous high-voltage current that heats the needle between 140 and 176 degrees Fahrenheit.
- Pulsed: Short bursts of high-voltage current with phases of rest. Pulsed RFA needles usually heat up to about 107 degrees Fahrenheit.
- Water-cooled: The needle is heated up to 140 degrees, but is cooled by a continuous flow of water. Water helps to regulate the flow of the current and prevent overheating of the needle.
Conventional and pulsed methods are great for small, well-defined lesions. The water-cooled method creates larger lesions. Talk to your doctor about which method is best for your specific condition.
Recovering from RFA
After RFA, you will be placed in a recovery room for up to an hour. Medical professionals will monitor your vital signs and any post-procedure symptoms. You may experience numbness or a superficial burning after RFA. In most cases, you will be able to go home the same day, but you will need someone to drive.
In the first couple of days after an RFA treatment, you may need to use an ice pack to numb pain and reduce swelling at the injection site. Also, warm showers are preferred over baths. Likewise, you may need to rest a few days before returning to your normal activities.
Pain relief usually starts a week or two after RFA. As your symptoms subside, your doctor may recommend physical therapy as part of your rehabilitation.
Is Facet Nerve Ablation Right for You?
There are plenty of degenerative disc disease treatments available to relieve pain. So when should you consider facet nerve ablation? A good indicator is when conservative treatments don’t seem to be helping. Facet nerve ablation can be a great alternative to surgery or, at the very least, delay surgery to accommodate your busy lifestyle.
Ready to learn more about this procedure and how it can help you? Our doctors at Orthopedic & Laser Spine Surgery use the latest research, technology, and treatments to reduce or eliminate your pain.
Schedule a consultation today by calling (855) 853-6542. By answering a few simple questions right now, we can start the process of managing your pain and spinal issues.